Single Tooth Replacement: Fixed Partial Denture Versus Single Tooth Implant
Reference: Balshi TJ, Wolfinger GJ: Single Tooth Replacement: Fixed Partial Denture Vs Single Tooth Implants. Valley Forge Dental Journal, Spring 1997.
Click Here for Article In PDF to View Slides
 There are many patients who present with the chief complaint of a single missing tooth. In the anterior region, single tooth loss is most commonly a result of a traumatic injury or it is a congenital anomaly. Single missing posterior teeth are usually caused by advanced caries or a failed endodontic procedure and occasionally by a congenital defect. There are several options available for the replacement of a single missing tooth.
There are many patients who present with the chief complaint of a single missing tooth. In the anterior region, single tooth loss is most commonly a result of a traumatic injury or it is a congenital anomaly. Single missing posterior teeth are usually caused by advanced caries or a failed endodontic procedure and occasionally by a congenital defect. There are several options available for the replacement of a single missing tooth.
A removable partial denture is one option for the replacement of a single missing tooth. However, most patients are not satisfied with this alternative due to the bulk of metal and acrylic and the unsightly clasps necessary to stabilize the prosthesis. While some may feel that a resin bonded prosthesis (Maryland bridge) is a viable option, clinical experience has shown that these resin bonded pontics do not have a good long term track record if the teeth are not prepared aggressively enough for mechanical retention.
Today, the two most common treatment options for single tooth replacement are the fixed partial denture (three unit bridge) and the single tooth implant. This article will discuss the advantages of a single tooth implant replacement over the use of a fixed partial denture and the factors to consider when treatment planning for single tooth replacement.
Single Tooth Implant Versus 3-Unit Fixed Partial Denture
Although there are many articles in the prosthodontic literature to support the use of a 3-unit fixed partial denture, it appears that single tooth implant replacement may be a more viable option for patients today. Some of the advantages include improved esthetics, improved hygiene accessibility, osseous preservation, and reduced future maintenance — all at a comparable cost. The replacement of a single tooth using an osseointegrated implant stems from an evolution in concepts, technology, and clinical applications, following years of basic research and fundamental studies. The method of osseointegration, developed by Brånemark et al, is well documented . Over a decade ago, Adell et al described the successful use of multiple osseointegrated fixtures supporting fixed partial prostheses in both maxillary and mandibular arches . Extrapolation from the original clinical methodology soon led to the successful treatment of partially edentulous patients. Clinical success in treating both fully and partially edentulous patients with osseointegrated implants ad modem Brånemark led to their use for the replacement of single missing teeth. This clinical application began in the 1980’s and was introduced to the literature by Jemt in 1986 . Lekholm and Jemt described the initial concept of single tooth treatment for patients who needed prosthetic replacement predominately to improve esthetics where a space or diastema existed, or to replace a missing tooth where the adjacent teeth were intact . A recently published prospective, five year multi-center study on osseointegrated implants for single tooth replacement, showed a 96.6% success rate in the maxilla and a 100% success rate in the mandible . From over 31 years of clinical experience with osseointegrated dental implants, there is no reason to believe that these single tooth implant prostheses will not provide these patients with a lifetime of functional service.
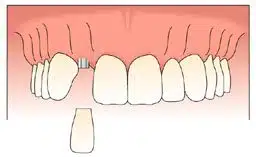
The esthetic advantage of a single tooth implant versus a 3-unit bridge is most apparent. A pontic for a 3-unit bridge simply sits on top of the soft tissue, whereas a single tooth implant restoration emerges from the soft tissue, providing a more lifelike replacement for a single missing tooth (Slide 1).
When replacing a single missing tooth where diastemas are present, it is difficult, if not impossible, to create an ideal tooth replacement using a fixed partial denture. With a single tooth implant it is easy to achieve an acceptable esthetic result (Slide 2).
Hygiene accessibility becomes a major issue when comparing these two replacement options. When a single tooth dental implant restoration is fabricated, the patient can easily floss in the conventional fashion as with a natural tooth (Slide 3). Whereas with a 3-unit fixed partial denture, the patient will need to use either a proxybrush, floss threaders, or superfloss to gain access beneath the solder joint area for proper oral hygiene.
When a natural tooth is extracted and not replaced with an implant, it is common to see an osseous defect occur. This osseous defect is often a result of the collapse of the buccal plate due to tooth loss and its functional stimulus. If an osseointegrated implant can be placed on the day of tooth extraction, the osseous contour can be maintained to provide a more esthetic appearance. If the implant is placed at a later date, it may be necessary to augment the osseous defect, using bone regenerative procedures either prior to, during, or after the surgical placement of the dental implant (Slide 4 & 5).
While we have had limited success in resolving osseous defects prosthetically, as part of a 3-unit fixed partial denture, it is much more predictable to achieve an acceptable esthetic result using a surgical approach. A surgical approach for bone augmentation can be done in conjunction with a fixed partial denture, however, when doing it with the surgical placement of a dental implant, it does not necessarily require an additional surgical entry. Having the ideal gingival contour provides the framework necessary to fabricate a most esthetic restoration.
When evaluating the cost involved for a single tooth implant versus the cost of a 3-unit bridge, it is important to note that there is a negligible difference between the two. An evaluation of fee schedules indicate that the single tooth implant restoration is slightly more expensive than the 3-unit bridge (a difference of a few hundred dollars). However, if the patient requires endodontic therapy, and/or post and cores on either or both abutment teeth, the cost of the 3-unit bridge becomes substantially higher. Insurance company statistics indicate a limited long term survival rate for 3-unit fixed partial dentures, which is evident by the fact that they will pay for a new fixed bridge every five years. If a patient requires a new fixed bridge every five years, for the remainder of their lifetime, this could become an expensive proposition, especially for a younger patient.
In addition, the future maintenance on the adjacent teeth, which may include periodontal, endodontic, or restorative procedures may be costly. These procedures may not have been necessary if the teeth had never been prepared in the first place for a fixed partial denture. Obviously a single tooth implant restoration, by its very nature, limits future maintenance procedures and creates a less complicated situation if and when problems do arise.
While to some, placement of a dental implant may be considered an aggressive approach, in reality, it is a most conservative approach from a biological standpoint. Placing a dental implant in bone provides a functional stimulus to help preserve the remaining bone and prevent resorption while preserving the enamel and dentin of the adjacent teeth. This approach is also more friendly to the pulp of the adjacent teeth.
In summary, the use of osseointegrated implants has evolved clinically from the successful restoration of fully and partially edentulous patients ad modem Brånemark, to the single implant supported prosthesis. This concept has many biological advantages over traditional prosthodontic methods including preservation of the natural dentition and supporting periodontum. Additional benefits include improved esthetics, improved hygiene accessibility, and fewer long term costs. A single tooth implant restoration should always be considered as an option when treatment planning a single missing tooth.
Slide 1
Patient presented missing both maxillary lateral incisors. Tooth # 7 has been replaced using an osseointegrated implant; and tooth # 10, utilizing a pontic of a 3-unit bridge from 9 to 11.
Slide 2
Replacement for maxillary lateral incisor tooth #7 using a single tooth osseointegrated dental implant, preserving the natural diastemas necessary for proper esthetics.
Slide 3
Single tooth implant replacing maxillary canine showing hygiene accessibility with convention flossing.
Slide 4
Osseous defect resulting from traumatic injury of maxillary central incisor. Tooth is shown with replacement using an acrylic tooth on a removable partial denture.
Slide 5
Photo taken immediately following stage II surgery, where the osseous defect has been treated with autogenous bone graft which has filled in the defect area, providing a nice gingival contour for esthetics around provisional crowns (#8 & 9).
References:
Brånemark P-I, Zarb GA, Albrektsson T. Tissue-integrated prostheses: Osseointegration in Clinical Dentistry. Chicago: Quintessence, 1985.
Adell R, Lekholm U, Rockler B, Brånemark P-I. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981:10:387-416.
Jemt T. Modified single and short span restorations supported by osseointegration fixtures in the partially edentulous jaw. J Prosthet Dent 1986;55:243-247.
Lekholm U, Jemt T. Principles for single tooth replacement. In: Albrektsson T, Zarb GA (eds). The Brånemark Osseointegrated Implant. Quintessence, 1989:117-126.
Henry PJ et al. Osseointegrated implants for single tooth replacement: A prospective 5-year multicenter study. Int J Oral Maxillofac Implants 1996;11:450-455.